So You’ve Found Your Kid a Psych Bed. Now What?
What does a one-week psych bed stay get you in North Carolina?
Turns out, it’s a few bottles of medicine and about a paragraph of “insight” into one of the worst periods in your life.
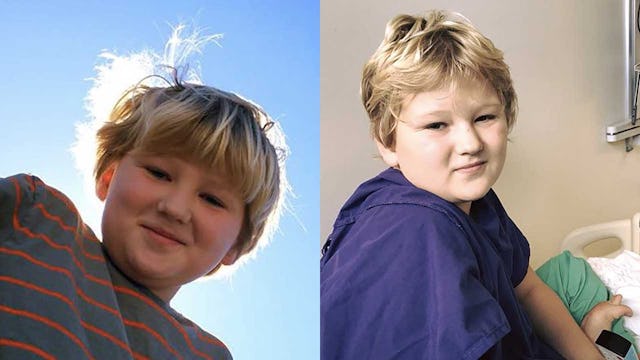
When my husband and I dropped our son off three hours away from home at a psychiatric hospital, following his psychotic break at school and the ensuing 256-hour wait for it, we were nervous, exhausted, and incapable of keeping from crying. Liam had made the trip via sheriff, and we followed behind, trying to keep our mind off things by listening to The Dollop podcast.
We had a short 10 minutes with him, where he begged us not to leave through red-rimmed eyes, purpled from lack of sleep and anxiety. I promised him I would send him a letter every single day, reiterated how much I loved him, and went through the same dialogue we’d had two dozen times since his break.
Him: “This feels like a punishment.”
Me: “It’s not a punishment, it’s a consequence. You remember why you’re here.”
Him: “Yeah.”
Me: “We want to help prevent what happened at school from ever happening again, right?”
Him: “Yeah.”
He was so brave. He’s never been much of a crier; he’s always seemed more concerned with maintaining his own schedule than emoting in any way. But I saw him cry more over the last 10 days than I’d ever seen before. And not fake tears. Real tears, coursing down his cheeks and making his eyes go puffy.
We signed all his paperwork in a blur, and found ourselves blinking in the parking lot staring at each other.
This kid has never been at sleepaway camp. He’s stayed the night a handful of times at the homes of friends and family, and only ever with parents who understand his limitations and have kids of their own on the spectrum or other challenges. He wasn’t allowed his comfort items. Everything was treated like a potential suicide tool. No staples. No hardcover books. No strings.
I get this. I understand that precautions have to be taken. I understand that the safety of other children is paramount as well as the safety of staff. What I don’t understand is the completely emotionless approach to parents. I felt like I was signing him off to jail, not to a place where he would get help. Phone calls were limited to twice a week, for 5 minutes, and visits to 20 minutes on Sundays. If there’s anything I’ve learned during the last month — and really, the last 11 years — it’s that helping children with mental illness is a group effort.
But this facility in Jacksonville didn’t ascribe to this thought. In the last three weeks, I’ve been running Liam around from doctor’s appointment to doctor’s appointment, following up with psychiatrists and his pediatrician, not to mention trying to figure out what to do. He was given the wrong kind of medication prescription from the facility, and he couldn’t stop throwing up for three days. Thankfully our pediatrician realized the error, the same day the facility called me to say that he had above normal liver levels and couldn’t help me directly. Then we discovered he’d been given too many different kinds of medicine at once and had to taper off one and increase another. We’re just trying to tread water until he starts at his new facility in two weeks, but every day is a close call.
The short story is that while at the psychiatric facility, Liam was given a heavy dose of antipsychotics, sobbed on and off the whole time, and was then sent home. According to their observations, he’s stable. They spent an entire week with him, and our discharge took four minutes.
I sent letters every day, sent them overnight, and he didn’t get a single one until the day before he was discharged. We didn’t find out until after five days that some of his clothes were not accepted by the staff, and he’d been wearing the same shorts (now full of holes) since admission. Books we requested for him never made their way into his room. What few creature comforts he was allowed were completely unreliable.
A few of the care coordinators were helpful, but the vast majority of the staff we interacted with on the phone made it clear that we were the enemy.
Not Equipped
My husband and I came to a realization not long ago (but probably too long, considering) that in spite of our education, our effort, and our love for our son, we’re simply outrun in terms of his mental illness, most specifically his DMDD. DMDD is a relatively new indication within the realm of mental illness, and it stands for disruptive mood dysregulation disorder. I explain it to others, and to Liam, this way. He has a car. But he’s only got two ways to make it go. He can get it to move at a crawl with a tiny bit of gas, or he can put the pedal to the medal. For Liam, the pathway from anxious/nervous/excited to furious/inconsolable/rage is a short and treacherous one. And it can show up at any minute.
We are in an abusive relationship with Liam’s mental illness. But in this case, he is our child. We don’t get to walk away; we don’t want to walk away. The clay isn’t yet set with him. He’s still becoming a person. And sometimes, I honestly think he doesn’t know what he’s doing, he’s so exhausted from constant anxiety and executive functioning challenges.
This is why we made the call to take him to the ER. Because we needed help.
I’m his mom. I’m always going to be his champion. He doesn’t often understand the decisions we make, and feels as if we’re punishing him when we’re in fact helping him, but he has learned that I will stand by him no matter what. When he called me from the facility, choking through sobs, he said in a tone I’ve never heard before, “Mom, I just miss you so much.” He didn’t know he was capable of missing me, this person he’s probably assumed was just along for the ride because I happened to give birth to him.
Is that a lesson for him? Hell if I know. He’s terrified of doctor’s offices now. Getting him through a single visit to his pediatrician was a Herculean effort. He says he loves me more often, sure. But he is still struggling every single day. Sometimes it’s a minute-by-minute play, and we just can’t predict the outcomes. That’s not worth the swap.
We had hoped for help.
We had hoped for compassion.
What we found was more discouragement and further reminders that this journey is just beginning.
Was it worth it? No. The psych bed was, by and large, a waste of time. Not every facility is like this, but the system gives parents absolutely no choice. It’s unfathomably horrible, a system in which sometimes 200 kids are vying for a single psych bed, only to come out drugged and sick and confused on the other end.
We certainly had no illusions that this would be a cure-all. But we did think we would have more insight into our child. Clearly the focus is not on treatment but on “stability” (which is certainly hard to quantify).
Somewhere Only We Know
One of Liam’s favorite bands is Keane (try explaining to him that the band is on hiatus, and you’ll hear his theories). The song “Somewhere Only We Know” may be their greatest hit, but it’s also the one that defines my relationship with Liam the most.
The truth is, for parents and families with children suffering with mental illness, the situation is something only they know.
During this whole debacle, people have said to me, “I just can’t imagine.” I understand they mean well. But I do imagine it. I live it. Every single day. Every phone call is a potential emergency. Every new side effect a concern. Every night it’s talking myself down from panic, trying to push aside the absolute worst fears that aren’t even unrealistic.
If I have learned anything through this experience — which is far from over — it’s that I am not alone. There are so many other parents and families out there who feel isolated, afraid, and just plain exhausted from the everyday fight.
Our health care system in the United States is an embarrassment. Colleagues of mine across the world are aghast that children should be treated this way.
I know it isn’t an easy fix. I know there is “work to be done” as people so often remind me.
But it is unacceptable that we’ve come to this point. We. Are. Failing. Children. Of all walks of life. Of every race and creed and economic background. And especially those without resources like my family has, with the constant worry of losing jobs or not being able to make ends meet. What I saw at Liam’s facility was simply preparation for incarceration.
Enough.
Teach Your Children
We have been so blessed in our lives to have the Hope Creek Academy family for the last four years. When I was speaking with someone from the North Carolina Hospital Association a few weeks ago, what I’d been trying to say about Liam’s school for so long finally came out of my mouth: Hope Creek Academy gave my son a childhood. Something that is taken from so many kids who struggle like he does. The struggle through public school can be so exhausting — physically and emotionally and spiritually — that by the time it’s all said and done, the joy is gone.
We didn’t stop a psychotic break. We didn’t cure his mental illness. But we have given him, and will continue to give him, understanding. From teachers who take the time. From students who have been there. From an extended family of parents who have walked in our shoes.
We can’t fix the health care system. But we can build more schools like Hope Creek Academy and the Wright School. We can give them more funding to reach more kids and help those who can’t afford tuition get the help they need.
My advice to you is to find your tribe. Find the people who understand. It won’t always be family, and they won’t always be near. But we need the support. We need to come together and demand better education and health care. These children are only children for such a short time, and they are amazing but fragile beings.