This Is What Life With Long COVID Is Really Like
When Keisha Kokonezi got sick in March 2020, no one had yet heard of Long COVID. Back then, we knew next to nothing about the virus which has killed millions. We believed it was solely a respiratory disease. Turns out, we were wrong. We believed it was surface transmissible. Wrong again. Arguably worse than all of that, we believed a COVID infection had two outcomes—survive or not. Yet again, we were wrong.
We hadn’t yet learned about the nightmare that is Long COVID. Nor had we realized exactly how big of a health crisis it would soon become for untold numbers of folks.
Keisha Got Sick With COVID In March 2020
In March 2020, Keisha knew COVID existed. She’d heard about the first infection in the United States and was worried that the virus would spread rapidly. But when her wife, Natasa, got sick neither of them believed it was COVID.
“We were a bit in denial about it,” Keisha told Scary Mommy in a phone interview. Which makes sense. Few of us realized COVID was here when we were told it was here.
Keisha got sick about a week after Natasa. Her condition began deteriorating when her wife was admitted to the hospital and Keisha wasn’t allowed to see her—no doubt the stress exacerbated her worsening health.
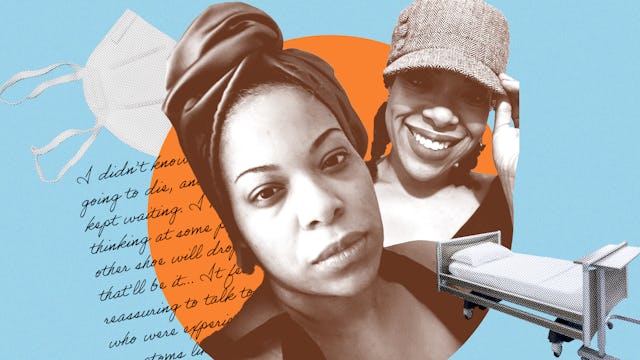
Courtesy of Keisha Kokonezi
She never experienced the so-called usual COVID symptoms—cough, fever, loss of taste and smell. Instead, her symptoms were largely gastrointestinal. She suffered from severe fatigue, numbness in her arms and legs, a feeling like her body was on fire (though she never had a fever), and an inability to eat for about two weeks because her body completely rejected food.
By the time Natasa returned from the hospital, Keisha could barely crawl out of bed.
She went to the emergency room. There, the doctors all agreed she had COVID, but her tests were consistently negative—likely because her symptoms had come on weeks prior and because testing protocol and accuracy was questionable.
Mentally A Scary Time
By the end of May, Keisha still wasn’t better. She was mostly bedridden, suffering from high blood pressure, heart palpitations, sweating, dizziness, insomnia, feeling as if her chest was seizing, as if her body was forgetting to breathe without conscious thought on her part. At one point, she lost the function of both of her hands for a period of days.
The biggest challenge for Keisha was food. Every time she’d eat, her whole body would shut down. She’d be unable to move or breathe easily until the food started to move through her system, almost as if her body could only do one function at a time.
Keisha recalls the worst experience was after taking three sips of Ensure—a meal replacement drink meant to add calories to her diet. After three sips, her body shut down.
“I didn’t know if I was going to die, and I just kept waiting. I kept thinking at some point the other shoe will drop and that’ll be it,” Keisha says.
During all of this, the emergency room doctors told her there was nothing they could do. They sent her home.
A Long COVID Rollercoaster Of Recovery And Relapse
By July and August of 2020, Keisha was recovering. She was able to get outside, take walks, do mild physical therapy. She wasn’t herself, but things were looking better. Then, a busy afternoon led to a massive crash. That relapse lasted until about October.
By then, long COVID had entered the conversation—if not on a national level, then at least on social media. Through a Long COVID support group, Keisha found others who were dealing with similar symptoms.
“It felt reassuring to talk to people who were experiencing symptoms like mine,” Keisha recalls, not only because the doctors she was seeing were making her feel as if she was imagining her symptoms.
Keisha was fortunate to enjoy a decent holiday season. Then April 2021 arrived, and everything crumbled. Keisha saw a new doctor who prescribed a change in supplements and medications. By the end of April, Keisha wasn’t able to walk. She couldn’t brush her teeth or do the most basic of things. She recalls an episode when in the middle of the night, she couldn’t lift her arm to tap her wife on the shoulder to say she needed help.
When she started twitching, she was finally admitted to the hospital. What followed was a short stay, followed by a seemingly unending rollercoaster of recoveries and relapses.
In July, another vicious relapse had Keisha suffering from temporary periods of paralysis. At times, she could only communicate via code—”wa” for water, “f” for food.
Gaslighting By The Medical Community
Courtesy of Keisha Kokonezi
At nearly every turn, Keisha was turned away, disregarded, or mistreated by the medical industry.
She recalls a psychiatrist who told her that her extreme fatigue after trying a new medication was “all in her head” and also a physical therapist sent by the hospital who terrorized her. The therapist, who didn’t understand Keisha’s condition at all, pushed Keisha’s body beyond the limits of its current capabilities.
After the therapist left, Keisha developed non-epileptic seizures. Her first lasted seven hours.
Fortunately, there were bright spots, and they’ve made all the difference. A switch to Cornell introduced Keisha to a doctor who listened and showed true empathy. That’s when things began to turn around.
Life With Long COVID Today
In an email, which Keisha wrote with the help of her wife, she summarized her diagnosis. “After Covid I developed Long Covid, Chronic Fatigue Syndrome (CFS), histamine intolerance, Mast Cell Activation Syndrome, dysautonomia, Functional Neurological Disorder/limbic impairment (wires in my brain got all mixed up basically), GERD, Psychogenic Non-Epileptic Seizures (PNES), and my thyroid antibodies are high.”
Keisha is still home bound — she hasn’t been for a walk since October 2020. She can sit up and she’s working toward standing. Her recovery has been helped by engaging in extreme rest, heart rate monitoring, tracking her diet and adjusting, if and when needed, cutting out all supplements (which Keisha learned negatively impacts her for reasons no one understands yet), and daily meditation.
With the help of a Lorrie Rivers, a CFS sufferer who shares her recovery with others, Keisha has learned about the importance of pacing your energy in CFS. It “has helped more than anything,” Keisha says.
Courtesy of Keisha Kokonezi
A Devoted Wife
Throughout it all, Keisha had friends and family by her side. A good friend of the couple’s began a GoFundMe, which raised and is raising money to help with medical expenses, and others have stepped up to help.
No one has stepped up more than Keisha’s wife, who Keisha names as “a huge part of my healing journey.” Between the sleepless nights and endless caretaking tasks, Keisha is aware that her illness took a toll on Natasa.
She wrote, “I couldn’t have gotten anywhere without her unfailing love, care and commitment to my recovery.”
Keisha is slowly getting better though she knows the road ahead of her is long. “I’m grateful for every second of this life I’ve been given, and even with everything that’s happened there’s a purpose for everything and purpose for me.”
Keisha’s story is one of suffering, but also one of hope—hope that recovery is possible, hope that better days are ahead, and hope that sharing her story will bring awareness to the untold numbers suffering from Long COVID, who need someone to listen, who need someone to understand.
This article was originally published on