Many Long-COVID Patients Are Struggling With ME/CFS Symptoms
The tragedy of COVID is often measured in terms of lives lost. Over 500,000 as of this writing. It’s staggeringly hard to wrap your mind around that number of empty chairs at the kitchen table, that number of grieving families and friends.
But an often overlooked measure of the tragedy of COVID is with respect to long COVID, wherein folks who were previously infected with COVID are experiencing symptoms for weeks or months after their initial infection. In many cases, the symptoms are so debilitating that people suffering from long COVID cannot return to their normal lives and activity levels.
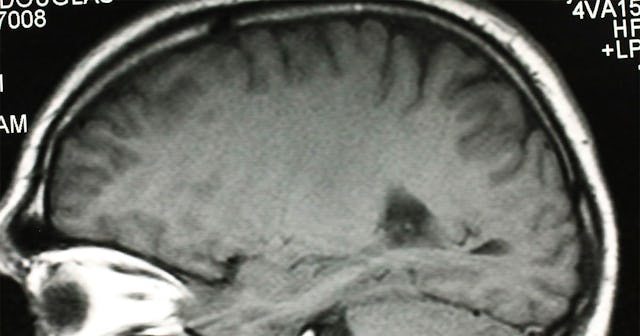
Two of the most common symptoms long haulers experience are fatigue and cognitive impairment, known more informally as “brain fog.” Researchers don’t know why some folks are experiencing these lingering effects, but a new theory is exploring the link between long COVID and brainstem dysfunction.
If that sounds scary or intimidating—it is. Brainstem dysfunction is related to chronic pain, migraine, and myalgic encephalomyelitis, also known as chronic fatigue syndrome (ME/CFS)—life altering diagnoses that are really devastatingly serious.
COVID Is Not Just A Respiratory Disease
Early on in the pandemic, COVID was considered largely a respiratory disease affecting the lungs. We’ve since learned we were wrong. COVID can impact every organ in the body, including the heart, kidney, and brain.
COVID enters human cells via ACE2 receptors thanks to its spike protein. “The spikes of SARS-CoV-2 are the crème de la crème: By the luck of the evolutionary draw, they are able to easily grab hold of protein gates on human cells known as ACE2 receptors and, like jackknives, pry these gates open,” according to an essay in the Summer 2020 issue of UCSF Magazine.
ACE2 receptors are found throughout your body—in your nose and throat, but also in your heart, your digestive tract, and in your brainstem, “which has a relatively high expression of ACE2 receptor compared with other brain regions.”
COVID Is Likely Neuro-Invasive
Westend61/Getty
While it’s still unclear whether COVID long haul symptoms are a result of the virus invading the brain or a result of inflammation due to your body’s large-scale immune response to the virus, researchers have found preliminary evidence that COVID-19 is neuro-invasive. Meaning: the virus itself is invading the brain and the nerves near the brain.
One of the most common COVID symptoms—loss of smell—is actually evidence of the virus’s neuro-invasiveness; the nerves that allow you to smell are directly connected with the brain. But loss of smell isn’t the only symptom with a connection to the brain stem.
Brainstem Functions Overlap with Long-Haul COVID Symptoms
Researchers have noted that functions of the brain stem—including those responsible for maintaining cardiovascular, gastrointestinal, and neurological processes—correspond with symptoms of long haul COVID in many ways.
Many COVID long-haulers, about 20-40%, experience chest pain, heart palpitations and tachycardia, or rapid heartbeat. Many of the neurons involved in respiratory and cardiovascular function, including those that regulate heartbeat, are found in the brainstem.
Likewise, neurons that control processes in your gastrointestinal tract are found in the brainstem. Dysfunction in this part of the brain stem can lead to a variety of issues including diarrhea, stomach pain, and vomiting. About 25-30% of long-haulers experience these symptoms.
About 20-70% of COVID long-haulers report some type of neurological symptoms, including fatigue, insomnia, and brain fog. The neurons that control your sleep-wake cycle, that are responsible for taste, and even those that are implicated in things like anxiety, depression, fatigue, and pain perception are found in the brain stem.
Brain Stem Dysfunction Can Be Debilitating
skaman306/Getty
During a webinar on COVID-19 organized by the International AIDS Society in July, Dr. Anthony Fauci, the country’s top infectious disease expert, noted that the symptoms many long haul patients are experiencing are “highly suggestive” of ME/CFS.
ME/CFS is life altering. The CDC recognizes that, “People with ME/CFS are not able to function the same way they did before they became ill.” The disease makes it difficult to work, to go to school, or to participate in family and social activities.
When it comes to COVID, even a mild infection could result in long-term, devastating consequences. A Germany study looking at 42 patients with persistent fatigue six months after a mild COVID infection found that: “Most patients were moderately to severely impaired in daily live.”
Brain fog can be similarly life altering. In a Q&A with Health Matters, a publication from New York Presbyterian Hospital, Dr. Alexander Merkler, an assistant attending neurologist at NewYork-Presbyterian/Weill Cornell Medical Center, noted that people suffering from brain fog experience memory loss, difficulty finding words, trouble with attention, and being overwhelmed by simple tasks. He notes, “A lot of these patients have not had any stroke or infection of the brain, no seizures or anything that was neurologically obvious during their COVID infection, but they’re coming away with a disturbance in their cognition.”
When something impacts the brain, it impacts you in a way that affects everything from the way you breathe to the way you speak. Your brain is you—it’s the collection of your memories and your reactions to jokes, it’s the words you choose and the very thing that makes you you beyond the physical things one can see. I’ve seen firsthand how an invisible (to the eye) disease can invade the brain and steal a loved one out from underneath your watchful gaze. It’s devastating–for the patient and the caregiver.
Our knowledge of COVID is constantly changing. Researchers are learning more with time. But the one constant has been that we don’t know what we don’t know. And as a result we need to focus on what we do know. What we do know is that listening to public health experts, social distancing, and wearing a mask work to prevent infection with a disease that could upend your entire life.
Information about COVID-19 is rapidly changing, and Scary Mommy is committed to providing the most recent data in our coverage. With news being updated so frequently, some of the information in this story may have changed after publication. For this reason, we are encouraging readers to use online resources from local public health departments, the Centers for Disease Control, and the World Health Organization to remain as informed as possible.
This article was originally published on